More memories, untold stories, of working nights in the ER.
I have fond memories of the staff I worked with for decades and shared many memorable experiences. They become your nighttime family, and a reason to smile when coming on shift. They put up with my handwriting and probably nurses who could read it better than me.
I remember the young lady, Room 7, night shift , with an abscess on her arm from shooting drugs. I told her we would use a local anesthetic, drain and pack it, but she was demanding IV Morphine or Demerol. She even suggested a dose. I finished the procedure with the local and her consent but with loud eruptions. When discharged, she went through the waiting room shouting "He's a butcher". I was surprised that didn't seem to clear out the crowded waiting room. I contemplated going into the waiting room wiping bloody hands on an apron, yelling "Next".
Night shifts, I remember finally getting time to run into the breakroom at 4am for coffee, first having wanted a cup a at 7pm. Coffee has heated down to a thick black syrup. You start to make a new pot and get called out. One also develops a very large bladder from night shifts.
The local donut shop guy used to bring a box of pastries to the ER at 2am. You could grab a donut on the run. An energy boost. Two of my favorite police officers, Patrick and Jim, somehow used to always show up in the breakroom around that time. Our man was actually brought to our ER one night with a cardiac problem and rumor is he got exceptional care. There were whispers of "the Donut Man is here".
.
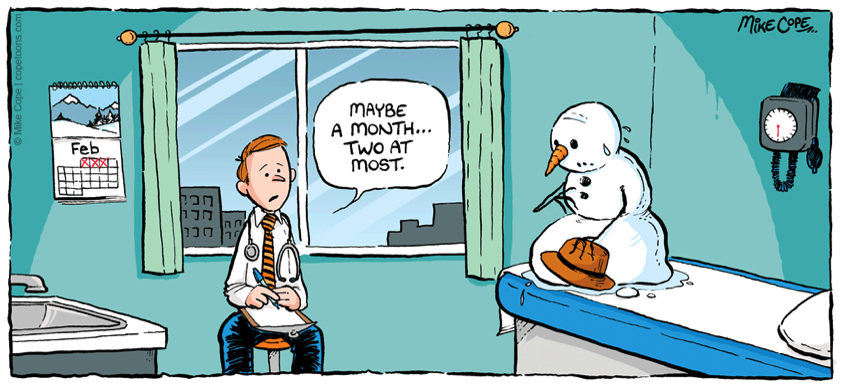
There is a show on TV now called “Untold Stories of the ER”. It’s ironic that after several decades of working an ER, the cases you remember most are not the gunshot, stabbing, auto accident victims, the countless resuscitations, the heart attacks, strokes, babies delivered. The most memorable are the unusual visits around 3am. One of my episodes might have the catchy title above.
It was a quiet night shift (never say that in an ER) and the next chart up was a lady in Room 9 with a chief complaint of something in her vagina. From experience I knew this could be anything, and I let my imagination wander for a moment. She kept saying "something". I figured I'd find out soon enough.
After the quick talk and exam, she was set up for a pelvic exam, draped, in lithotomy position. Mayo stand with instruments, next to me, I was on the little black stool with wheels. On exam the lady appeared to have a spray can lodged in her vagina. The spray tip was missing and the exposed plastic tube was lodged up behind the pubis, with some bleeding from her attempts to remove it. I had to push the can further in to dislodge and deliver it.
As I pushed, I apparently pushed on the plastic tube. The can discharged suddenly, blowing air and mist straight at me. I reflexly pushed away, and with the stool on wheels, flew back and hit my head on the wall. I fell off the stool and had grabbed the Mayo stand on the way down. That made a very loud crash sound. When I looked up at the nurse, she was just staring with a very unusual look on her face and her mouth open. She might not have even heard the can discharge and thought I was just emphatically done with the exam, The patient was draped and would have no idea what happened.
Soon there was a crowd at the door, like the entire ER staff. I shook it off, regained my composure although perhaps not my dignity. I got back to the exam, and delivered a spray can…a Medi-Quick spray can to be specific. I learned early on not to ask how or why or make judgements on the endless variations of human behavior that end up in the ER. Patient discharged relieved. The doctor had a tender bump on the back of his head.
We normally send anything we remove from a person's body to pathology. At some point they would have to wonder what we're doing in the ER... a soda bottle, a cucumber, a spray can.
Perhaps my favorite case in the 28 years. A busy night shift. Some pretty sick patients. Workups in progress. At 2 or 3 am there was a stat call to pedi floor. This was my first year at ST and I usually took an ER nurse with me, to help me find where I was going in the seven floor new hospital and to have someone with me I knew I could rely on.
A 6 month old boy was post op hernia repair and was in a crib on the pedi ward. The mom had elected to sleep in a chair next to her child. She noted a change in the baby’s breathing and called the nurse, and then the stat call. I found the baby with minimal respiratory effort and a bit cyanotic. Heart beat was present. A pedi bag with a small face piece wasn't at hand. I started mouth to mouth, or in this case to nose and mouth, and tried to get a history as to why he would stop breathing. I found pinned pupils. His chart had the order for MS IV PRN pain, and as the baby cried was given additional doses.
There was no Narcan on the floor and the ER nurse literally ran down to the ER for the med. The baby had pinked up with the mouth to mouth and now I was bagging the infant. On giving the IV Narcan, the baby aroused, cried vigorously and had a normal exam. I had quickly introduced myself to the mom when I first got there, but realized she was still standing next to the crib as we resusitated her son. In the ER we seldom have family in the room when working on a critical patient. I explained the situation to her, the pediatrician was on the way in to take over the case, and I got a stat call to return to the ER.
Fast forward a decade or so. A busy night in the ER, all the rooms full, waiting room full. I had seen all the roomed patients and workups were in progress. I was checking the stack of a dozen charts of patients waiting to be seen. One was a 10 year old boy with an asthmatic attack. On those busy nights like this I would sometimes bring patients back myself and put a chair in the hallway to get my evaluation started. Drove the nurses crazy, but they did it too. It always made me nervous not knowing how sick the folks waiting were when we had no place to put them. This boy seemed the sickest and I brought him back with his mother. I sat him in a chair, listened to his chest for the wheezes and ordered a breathing treatment. She said “You don’t remember me do you? Well I remember you.” She gave me a hug and reminded me of that night a decade earlier when her son was 6 months old, now a healthy young boy with a mild asthmatic attack. The case could have ended much differently if the mother had not stayed at the bedside.
Don’t forget to thank your ER Staff. They often see you on the worst day of your life. First responders and the ER staff seldom get much feedback on patients they resuscitate, bring back from the dead, and stabilize for admission. In that “Golden Hour” when life or death is in the balance, their actions, make the difference. Seldom are they able to follow the course of the patient after admission. Feedback is rare for ER crews, even more rare for the Paramedics, first responders, in the field, but it can happen.
I recall the first time I used the “auto transfusor”, a new device in ER’s for recovering lost blood from a chest tube and transfusing that blood back into the patient.
The ringdown was a stab wound to the chest, young male, pulse, BP lost in transit. He entered ER unresponsive with stab wound to upper left chest, no pulse, blood everywhere. This was before the ER technique for hypovolemic arrest and chest wounds was to open the chest in the ER to cross clamp the descending aorta and do open cardiac massage.
One dilema in the ER was when to call in consultant. You couldn’t call in the surgeon from home for a dead body. He was intubated, had two large bore IV’s. and a left chest tube that quickly filled the pleurovac with blood. I don't remember if we used the Mast Suit, inflatable compression pants that force blood from the lower extremities up into the central circulation. The nurses set up the auto transfusor and I tipped the pleurovac and poured the blood into the transfusor chamber. A little sloppy, not very planned out or sterile. We put his own blood back into him, as well as O neg and type specific from the blood bank. He’d had a several liters of NS as we waited for blood. We had gotten cardiac activity and a weak pulse back.
The surgeon oncall arrived and called in the OR crew. It was almost 7am. Sunday morning. I’d been working on the guy for over an hour. Fortunately not too many people had been waiting. But they couldn’t get a full OR crew, so as my relief arrived, I went into the OR to assist. My job was to squeeze blood bags into the guy, I think I got up to 7 or 8. When the surgeon cut open the chest, there was no bleeding, a bad sign. He found and repaired a laceration of the right ventricular outflow tract. I left the OR around 9am and got home and in bed by 10am.
That next shift, I called up to the ICU and was told the patient had survived and was stable. Somewhat of a surprise in view of the long down time. I was still worried he might have had some brain damage. I didn’t get any further follow up until the nursing supervisor wanted to talk to our crew from that night. She said the patient had done well, walked out of the hospital intact, but had accused us of stealing a ring and watch worth two thousand dollars. What I remembered about that night was that our crew started with a very dead guy and made him undead. Neither I nor the crew noticed any jewelry. We never heard anything more about it, but it seemed like a simple thank you for bringing him back from the dead would have been nice. We found out that he had been stabbed by his sister with a pair of scissors. As an aside, the stab wound was just below the left clavical. It is said that women stab in a downward action, thus the damage to the RV outflow tract. Men tend to hold the knife/blade differently and stab upwards.
Another untold ER story.
A Code 3 trauma ring down early am, per paramedics, stab wound to abdomen, head injury, drugs, out of control and restrained . Patient brought in combative, under the influence of what was later found to be PCP, yelling loudly, incoherent, and was completely uncooperative, thrashing about. Trauma w/u started, IV in with difficulty, labs ordered. T&X. He had a scalp lacerations and large hematoma. Neuro exam was difficult with the PCP. He had about a two inch stab wound in the mid abdomen. A loop of small bowel was being pushed out as he strained. Difficult keeping him restrained, now in leather restraints. Before long about two feet of intestine has been pushed out like toothpaste. He had calmed down somewhat with IV Haldol, but we still had to be able to follow the neuro exam. The surgeon on call had been called, but remember, he is home in bed. The extruded intestinal loop became cyanotic due to entrapment in the small wound. I used a local, got my finger in the wound pushing against the bowel, attempting with a scalpel to enlarge the wound without nicking the intestine….or my finger. Thinking back, there must have been a better way to do this. I was able to enlarge the wound, the loop of bowel got blood supply back and color returned. We put a saline dressing over the loops of intestine. CT head ok, and the surgeon arrived, called in the OR crew and took him off our hands. When I say we in a case, I mean the trauma team where each member has done their tasks a thousand times. From the Paramedics, RN.s, Lab tech, Respiratory/EKG tech, X-Ray/CT tech, to the Clerks. Heard that the guy did fine.
Hard to forget the sight of the loop of small intestine oozing out and laying out on the guys belly. Think about that when you squeeze the toothpaste tube.
Here's one way to teach your teenager
the dangers of drug use.
When Emily was 16,
she spent a night shift in the ER with me.
The night was pretty mellow until there was a commotion at the front door of the ER. A car had driven up, dumped a young male on the pavement, and sped off. We got him on a gurney and into the trauma room. Emily stood in the corner of the room watching the resuscitation attempt. It was pretty obvious he was an overdose, no signs of trauma. He had no pulse or respirations and our team started CPR. The nurses got the IV in, Narcan in, I intubated him, we continued CPR with no cardiac activity on the monitor. Epi in and at one point it looked like fine V-fib and we shocked him several times, still no pulse and then flatline again. Emily remembers well when I “called it”. Time of death…. He was dropped off dead and he stayed dead.
Emily later told me she had felt nauseated, lightheaded, like she was going to pass out, especially when the young man was shocked and his body jumped. She said a nurse had gotten her seated with her head down. She also remembered that his “friends” had packed his genitals in ice, a street method of “treating” overdoses, an attempt to keep him breathing.
Later we heard the story that the patient had just been released from prison. He probably used his regular dose of heroin, but his tolerance had changed considerably, causing the overdose.
I suspect Em learned about the dangers of drug use that night.
Emily also has told me that’s the night she decided not to be a doctor. She has made a great teacher.
Random ER memories
What other job description can boast of
having been spit on
urinated on
stooled on
vomited on
bled on
having been grabbed, punched, pinched, scratched
having been confronted by a gun, a knife
First responders, police officers, prison guards
probably also qualify.
It seems that most of my memories of ER cases are the cases where adrenalin was involved. In the ‘Old Days’, before paramedics, patients arrived by EMT’s (Emergency Medical Technicians) . Basic CPR in progress, being bagged and pumped on. There were procedures we could do on arrival, intubation, IV meds, defibrillation. Not to demean EMT’s. They did well what they were trained to do and allowed to do. The generation before them was the ‘ambulance driver’, load and go. So the way the patient
presented to our doors changed considerably over my career with the advent of Paramedics. Another issue was that early on in my era, patients couldn’t be pronounced dead in the field, so they were bought to the ER even though obviously dead. As I recall the ring down for that was 1054, ‘possible dead body’.
When critical patients/CPR in progress (that ring down was code 3) arrive by a paramedic unit, usually they were intubated, IV meds/saline given, defibrillation attempts have been made if indicated. As an ER doc, I would continue CPR and any additional procedures or meds I could add to the mix, but often if the patient hadn’t responded in the field and the run to the ER, there wasn’t much more we could do but pronounce them after 20 to 30 minutes.
There were skills you had to be confident in performing quickly and successfully. Airway management, difficult intubations, cricothyrotomy, cardiac massage, central lines. You were the only doc in the house. If you needed a surgeon, cardiologist, internist, pedi, OB, they were at home asleep. If you called for a consult or admit, it would take at least 30 to 60 minutes for them to be on site. The ER doc needs to know the diagnosis and treatment of the urgent conditions in each of the specialties.
The first 4 to 5 years I worked at ST, there were no sleep in specialists. If a patient in the ICU crashed, the ER doc was called and you had to leave whatever you were busy with in the ER. You also got called if a ward patient fell out of bed, seized, became unstable, or had any other problem that might arise.
Between the ER and calls to L&D, I delivered over 100 babies before an OB doc started sleeping in.
Deliveries were usually a happy and uncomplicated event. Often folks come into the ER on the worst day/night of their lives. At least with babies, it’s a joyous event. The L&D nurses are fully competent to deliver babies, I'm sure much more so than me, but protocol was that they call the patient’s OB and the ER doc if a patient was in late labor and about to deliver. The OB was of course at home at sleep, so I got there first.
You rush in, introduce yourself, sit down to a crowning baby, do a quick episiotomy if necessary and guide a baby into the world. Sometimes a quick bulb syringe to the airway, stimulation, then a vigorous cry and pink baby. You cut the cord or if the Dad is present offer to have him do it. You record Apgar scores at 1 and 5 minutes. Putting a vigorous, healthy, baby in the mother’s arms was always special.
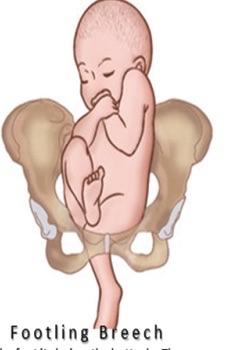
Unfortunately not all my OB experiences were like this. I vividly recall one call. When I came in the room, the patient was draped on the delivery table, and what I saw was a single footling breech. One leg of the baby presenting along with a prolapsed umbilical cord. The fetal monitor showed decelerations and therefore fetal distress and a critical emergency. Delivering a breech like this was near impossible, especially for me. They are safely delivered by C-Section. I was able to push the leg and rump back up into the birth canal and take the compression off the cord. The fetal heart rate went back up. I sat there for about 10 minutes pushing. The OB doc finally arrived and did the C-Section. I had to run back to the ER to finish workups, waiting list. I later called to find out the baby looked great.
Another memorable, but sad case was a 14 year old girl presenting to the ER with cc of abdominal pain. She was brought in by her parents. She was in a great deal of distress and we put her in Room 9. She was obese for a young person and had a large belly. The differential diagnosis would include appendicitis, ectopic pregnancy, trauma. On exam it turned out she was in late stage labor with a full term pregnancy. We didn’t have a chance to check for fetal heart sounds, as she was crowning and I delivered a vigorous baby boy within minutes of her arrival. She was upset and in pain, but when I presented her with the baby, she kept screaming, “that’s not my baby”. At this point I hadn’t cut the cord, so I was pretty sure it was hers. We got the girl settled down, IV started, labs drawn, OB & Pedi called.
I went to the reception desk and ask for the parents. My recollection is like it happened yesterday. We were standing at the desk and as I told them of their new grandson, the mother fainted and as I caught her, I heard the stunned father say, “but she doesn’t have a boyfriend”. The mom recovered, but I got called into a critical case and didn’t get to see the parents in the room with their daughter and new grandson. The girl had hidden or didn’t realize she was pregnant for almost nine months, That’s some denial. No prenatal care. Went through hours of labor before being brought to the ER. Incredible.
Because of the age of the patient, we notified Child Protective Services to investigate the circumstances of the child’s sexual encounters.
Like most of the cases and drama in the ER, we seldom get much feedback on patients admitted, so I can’t say how this baby was conceived, the good news was that it looked healthy despite the conditions of its gestation.
A memorable OB case involved one of the male nurses. Women in late stage labor would often present to the ER by car or ambulance. The ER nurses would triage the patients as to who had the time to be taken up to L&D versus those that birth was eminent and those patients would be kept in the ER and delivered there, to avoid a problem in the elevator for one thing. We kept the lady in the ER if I would have had to go up to deliver anyway. Specialist had to be awakened and talked into getting up and coming in for a 3am case. The ER admission desk was right around the corner from the doc’s work desk, so you could often hear the loud voices. We didn’t have a triage room at that time and a lady in very active labor presented at the desk. Her husband was pushing her in a wheelchair and one of our male nurses, I’ll call Able, went out to triage. Then I heard a loud:
“We’ve got hair!!”
. He had lifted the ladies dress and had seen the baby’s head presenting. It certainly was an important triage point and the lady was rolled into Room 9 and in short time, we delivered a healthy baby. But nurse’s loud triage proclamation stuck in my mind. Our usually crowded waiting room is adjacent to the admission desk. What if he had lifted up the dress of the wrong patient. I can’t help but smile when I think of lifting a lady’s dress in the hallway for triage, and it’s a phrase I can’t forget, “We’ve got hair!!” We eventually got a triage room.
Unfortunately, the most common use of room 9 was for miscarriages. (Rooms 2 & 9 had OB/Gyn exam tables)
It was a very common ER case. A pregnant lady, bleeding, checking for open os, tissue, CBC, Rh type, r/o ectopic or some other problem.
Term of pregnancy varied from tiny conceptus passed to near viable fetus.
One of the worst decisions is when is a fetus/baby is viable. Dates usually unreliable and usually it’s obvious, no signs of life. Early in my internship at VMC, I had a month rotation in the Neonatal ICU. A ward with rows of incubators. One of the babies I cared had a birth weight of less than 800gm, about 1 and a half pound, premie male. He looked more like a fetus than a baby. He had one crisis after another. Later in my internship I had another rotation in the NICU, the baby was still there, and he was one of my patients again. He’d been in that incubator for 5 months as I recall. Longer than he’d been in the womb. He did not survive. This was back in 1973-74 and the technology for keeping these premies alive was just developing. The debate was also going on as to when a fetus is viable based on weeks and weight. Will the extreme premie be normal in development? Sitting with the couple, you witnessed the emotional toll.
Another “Untold (more serious) Story from the ER”. It was like 1am and a code three ring down came in, MVA rollover, child with severed limb. She was brought into the Trauma Room, a young girl, I don’t remember, maybe an 8yo. Her left arm was severed just below the shoulder. A tourniquet controlled the bleeding. Paramedics said they couldn’t find the severed arm at the scene.
Trauma screen otherwise looked good except tenderness in the LUQ abdomen. Nurses, lab tech, X-Ray tech all working in a carefully coordinated routine - IVs, lab work, type & cross, X-rays.
We were maybe 30 minutes into the workup when a Highway Patrolman ran in carrying a couch cushion with an arm laying on it. We put it on ice and got the transplant service at Ralph K. Davies in San Francisco on the line. They would send a helicopter. It was eerie for all of us, seeing the child’s arm on a Mayo stand in the corner of the room. We continued the workup. She still had that tenderness in the abdomen, LUQ, over the spleen. We had had to medicate her for the pain & terror and that can obviously blunt the pain response and exam.
If we called in a surgeon, kept her for surgery for a ruptured spleen, she would loose the arm. If we put her in the copter she could possibly bleed out, die, from the belly injury. The tenderness hadn’t gotten much worse in over an hour and the copter was landing. I elected to send her, worried I could kill her by doing so. Moving on, I went out and had a dozen patients to catch up on.
I checked in with RKD the next day and found out they had successfully replanted the arm and she did turn out to have a laceration of her spleen which they also took care of. The good news, about eight months later, RKD sent a video down for our team. It showed a little girl moving her arm and hand very nicely. Our team celebrated, but thinking of the risk I took with her life is a moment I couldn’t forget.
Could have easily gone the other way.
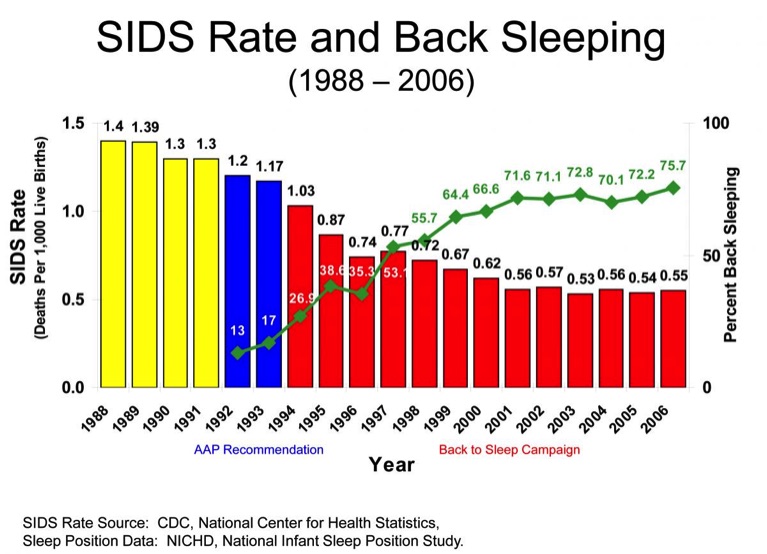
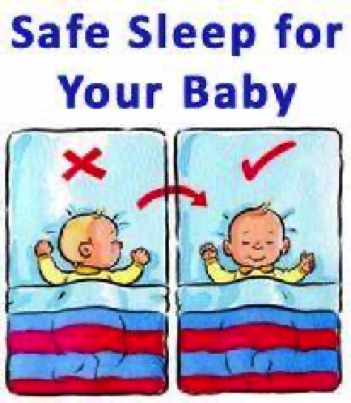
The graph shows the incidence dropped significantly over an 18 year period due to the emphasis on back-sleeping, the “Back to Sleep” Campaign, beginning 1994. Also avoiding loose bedding, among other precautions. The incidence in the 70’s was even higher and all to frequently seen in our ER.
Sudden Infant Death Syndrome, Crib Death
I recall a number of SIDS cases early in my career. Most time the parents would find their baby not breathing, sometimes cool to the touch if time had passed. One mother had her baby stop breathing as she held him. As I recall it was mostly in first born males, about 4 months old. There was seldom a successful resusitation in these cases, because the down time was usually long. Saddest time, of course any death, but perhaps the saddest was the SIDS.
Parents put a healthy baby to sleep and find him not breathing and usually beyond resusitation. Then sitting with the grieving parents trying to explain SIDS, as if that was possible.These cases would always take a heavy toll on the staff, often with tears. It was an all too common problem in the 70's and 80's. Fortunately the incidence of SIDS has dropped dramatically since the 90's when the "Back to Sleep" campaign started.
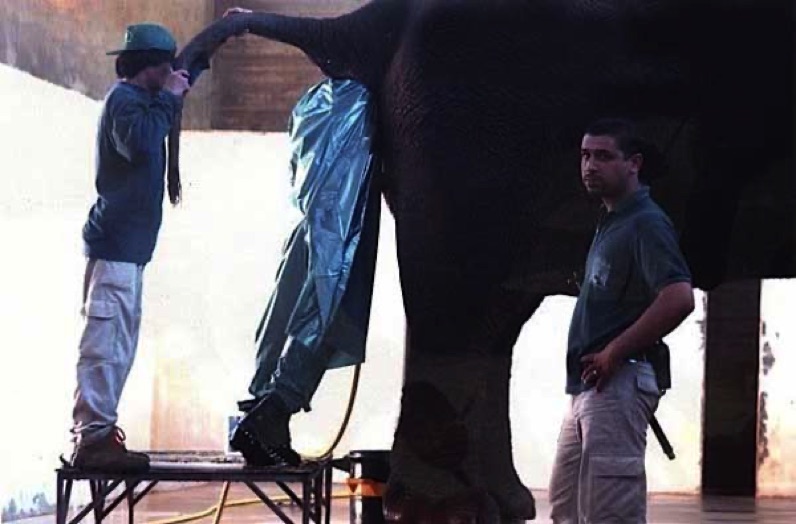
A Rectal Exam on an Elephant
Not my job, but brings up a lot of questions
Whenever you start thinking you have a unpleasant job, think of this guy.
So many questions!
Do you think he has a flashlight?
What kind of headgear does he have on?
What about the possibility of flatus?
Is that hose hanging down a breathing tube? A water hose? A safety rope?
Could he disappear suddenly?
Does he have a shovel?
How long can he stay in there?
Does he like his job?
How much less does the guy holding the tail get?
So many questions!
The Cucumber Guy
“Untold (and should probably remain untold) Stories from the ER”
Another memorable case was the guy with the very large cucumber in a place it didn’t belong. It was always hard to take a history in a case like this. Like: What’s there? How long’s it been there? No use asking how it got there, although I once had a guy that “fell on a soda bottle in the shower” and it lodged in his rectum. Talk about bad luck.
It was difficult to get the cucumber out, and the big question then was, should we send it to pathology or dietary. This guy actually came in sometime later with an even larger vegetable, and he had to go to Surgery to get that out.
There was a fellow that had a full two liter Coke bottle up his rear in such a way that you could feel the screw top up over the liver, RUQ. On rectal exam I could just touch bottom of the plastic bottle. The X-Ray was facinating. He went to surgery as well. I was told later it was Hawaiian Punch. It was a full bottle, I hope it wasn't served in the break room. Nice memory when I look at a 2 liter soda bottle.
Picture the call to the on-call surgeon at 3am asking for a consult and admission on these cases.
Not a good way to make friends.
Another fellow had a large vibrator that he’d taken its leash off.
I think he had waited until the batteries ran out before coming in.
Except for the spray can and my head injury pelvic exam, most women probably were able to remove their problems at home.
There were marbles once, cat’s eyes as I recall.
Retained tampon was probably the most frequent visit for retained foreign body.
I had a lady with a significant vaginal wall laceration near the cervix. She said it was because of the size of her boyfriend. He was at the bedside and when I looked at him he had this big grin on his face.
To top off my career, I was always hoping for a unit coming in with a couple on a gurney having gotten locked together during intercourse. The medical term being “Penis Captivus” usually due to “Vaginismus”. It’s in the literature, probably pretty rare, some say a myth, but something for you to think about next time………
Picture the 911 call on that one.
I hope I haven’t offended anyone with TMI, but some folks might be curious about what goes on behind the curtains.
What’s it takes to make a young nurse nearly vomit and pass out.
Another “Untold (sad & unfortunate)
Story from the ER”.
One night there was an elderly lady brought into the ER. I don’t remember what her chief complaint was, but her legs were swollen and her stockings were stuffed with tissues. I was unwrapping her legs when a cup or more of maggots spilled out on to the gurney and onto the floor. The young nurse, a float to the ER, wavered back against the door frame and put her hand to her mouth. She left the room. The lady had multiple stasis ulcers on both legs from poor circulation. By the way our regular ER RNs probably would have just scolded me for making a mess.
However, the maggots had kept the wounds completely debrided and clean. Actually maggots have been used in medicine for centuries. They consume just the necrotic tissue, and will debride a wound far more precisely than is possible in a surgical procedure, Secretions from maggots are believed to have broad-spectrum antimicrobial activity. In 2004 the FDA approved the use of medical maggots for wound care. In this case, it’s tragic that this lady’s level of attention and care allowed this to happen to her, that flies were able to lay eggs in her wounds in the first place. I don't know who got to clean up the maggots.
The ER is the always open back door to the hospital. As in the Chicago shooting, anyone can walk in for any reason. The staff is always under the possible threat of violence. I’ve been out of the ER for many years but some incidents are hard to forget. We would often get injured gang members from rival gangs. We’d try and keep them far apart, but several times open fights occurred. Gurneys overturned, nurses punched, pushed to the floor. I only got punched, kicked, threatened with a weapon, a handful of times in my career. I recall working on a gun shot victim and when we rolled him over a hand gun fell to the floor. We all just stared at it. We had a gang member pull a knife in the waiting room and demand to see the guy we were resuscitating from knife wounds.
Before we could restrain him completely, a guy high on PCP punched a nurse in the face. In those days, we had an unarmed maybe 60 year security guard. Nicest guy in the world but not someone who should be expected to control these situations. The police would respond but they weren’t able to be in the ER 24-7. One ploy we used was to have the donuts out at 2-3 am in the morning, usually got a unit to stop in for a bit. It was reassuring to have a couple uniforms in the coffee room. The ER is a unique place, no "appointments", no control over the front door. Actually one night we had a car drive through the doors. It can go from a “slow night” to ring downs, chaos in minutes. The ER nurses, clerks, techs are unique as well. They can adapt to the unpredictable pace, "blood and guts", which few can. I remember a case where I called for a consult on one of “those” nights.
The consultant’s line is hard to forget,
“I can’t work under these conditions”.
You could start a shift and 12 hours later, realize you hadn’t taken a break, hadn’t got into the coffee room all shift, and you badly needed to empty your bladder. Adrenalin was the caffeine. I can’t picture myself working in any other area. Working night after night with a talented reliable team that has become family. Good or bad, happy or sad, you got fairly immediate feedback on your treatment efforts
in the Emergency Department.
The Mercy Hospital ER in Chicago lost staff and a PD officer to a senseless, unpredicatable shooting. Unfortunately, somewhere, sometime, it will happen again.
I don't want to give an unbalanced view of the ER. For every case like above there are hundreds of times when a heart is restarted, a trauma victim is resuscitated, and gotten to surgery, the damage from a stroke is minimized, a chest pain or abdomial pain workup saves a life, and yes even the screaming toddler in pain at 3am with an ear infection. The rewards far outweigh the risks, but the risks are there.









Almost killed by a red balloon
Once upon a time, long, long ago, I was driving into work for the night shift. I had asked Cheryl if I could drive her brand new car to get a feel for it. I was driving down Summit Rd into the setting sun. I had the sun visor down. There was a pickup truck coming toward me and an arm was out the driver's window with something red in the hand.
All of a sudden there was loud explosion and I was covered with water, glass and bits of red stuff. There was a hole the size of a football in the windshield. The sun visor had been ripped off and was on the back deck, behind the back seats, with glass embedded in it. I got off the road and realized I'd had a red water balloon thrown at my car.
If I was going 50 mph and he was going 50 mph the balloon hit me at 100 mph. If the sun visor hadn't been down it would have hit me in the head and my head might have been in the back seat. Police report made, no action.
Lots of ways to get dead. Picture the obit. "Succumbs to Red Balloon".
I had to drive back home and explain to Cheryl the big hole in the windshield of her brand new car. Perhaps another way to get dead.


How tired can you get at work?
The medical personnel in this pandemic are pushing the limits.
There's an old tale going around: Nurse walks into a bank totally exhausted after an 18 hr shift. She grabs a deposit slip, pulls a rectal thermometer out of her purse, and tries to write with it. When she realizes her mistake, she looks at the flabbergasted teller and, without missing a beat, says, "Well, that's great...some asshole's got my pen."
I had several memorable Inappropriate Sleep Periods (ISPs) during my internship, I had clinic time after a 24 hour shift. I fell asleep while talking with a patient that I'd followed all year. She was a sweet elderly lady, and when I awoke, she was smiling. I was embarrassed and apologized profusely. She said she had let me sleep for 15 minutes, because I looked like I needed it badly. Not my best moment, but she was my favorite clinic patient..... I hope I didn't snore.
Another time I had finished 24+ hour shift as intern,
driving home fell asleep at stop light, left hand turn lane, signal.
Awoke to someone knocking loudly on the window and some honking.
I'm sure the people thought I was drunk at 8am.
I hope our heroes are able to get some rest and have the right protective gear. We have to keep them in this battle.

Emergency Room Moments
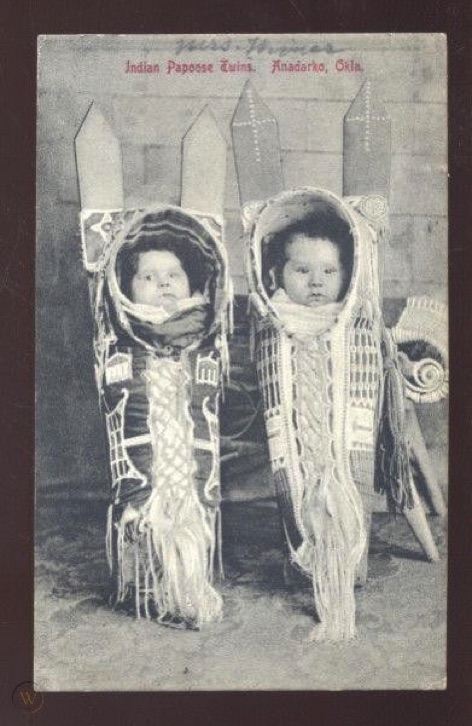
When we had to suture lacerations on an infant, toddler we would usually "papoose" them to control movement. Now they are sedated a bit with a nasal drop medication. Unfortunately in the old days, like 40 years ago, we didn't sedate, just a local was used, especially if it was a head injury, lac.
The children would obviously be upset, crying, yelling out. What they usually would yell out was all the swear words that were used in their household. This would often include the F word among others. If the parents had remained in the cubicle it was always amusing to look at the embarrassed expressions on their faces.
Here’s another memorable pelvic exam.
I needed to do a pelvic exam on a nice, grandma like older lady. She was all set up, draped in the lithotomy position. I saw she had what looked like a tattoo on her inner thigh. The skin was fairly wrinkled and I had to subtlety stretch the skin a bit to see what it said. To my surprise it said “Enter Here” with an arrow. I’d seen several interesting tattoos in this area, but this is my favorite.



ERs Don't Close for Holidays
I want to say Merry Christmas and all the best in the New Year to all of those first responders, paramedics, fire personal, ER personel, nurses and MDs, including those up on the wards. I've been out of it for a long time, but worked many, many holidays. As I recall, it seems like Thanksgiving and Christmas had lots of gall bladder attacks from the big dinners, pulmonary edema from too much salt, a few ETOH problems. New Years Eve is the worst, unconscious drunk patients, auto accidents usually with drunk drivers. It's a tragic part of the job to tell a family of a death. Injuries from falls, barroom brawls, knifings, shootings. And then there's also the regular visits as well, the heart attacks, CPR in progress, abdominal pain w/u, fevers, a w/u on a infant or child with a problem.
You have to get a good rest before, and usually after a shift one's ready to pass out.
Too often it's hard for the staff not to take tragic results home with them.
Not much time to celebrate with the family .
Merry Christmas and thank you for what you do.
I just read the stat that 240,000 children a year are brought to the ER for a toy related problem. That seems to be over 27/hour, over 657/day.
Please be careful with the little ones.


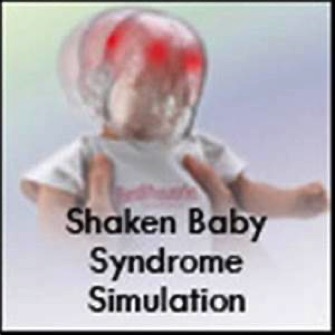
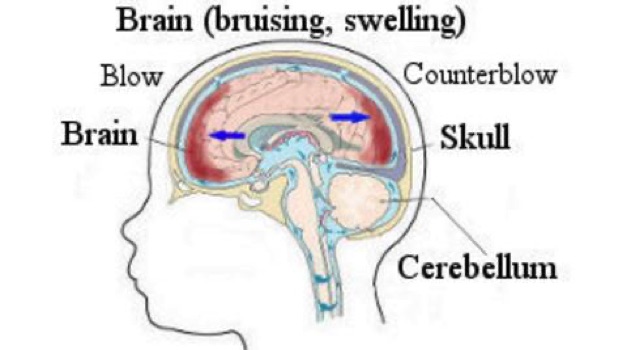
Shaken Baby Syndrome.
Baby brought in unresponsive, vital signs ok,
On neuro exam had retinal hemmorages.
Suggestive of SBS.
Father was sitting in hallway with a three year old or so on his lap.
I asked him if the infant had had any head trauma.
He said no. I asked about her being shaken somehow and he said just when she wouldn’t stop crying. I asked him how he shook her and he put his hands on the three year old and started a shaking motion. I stopped him before he did the shaking. He had no idea he could hurt a child that way.
Neuro came in and the child had head scans, admission.
Never got followup on if she left the hospital or if she did, what impairments.
My Spanish
A humorous memory of a nice older Hispanic lady in Room 1 with stomach flu, vomiting, a bit dehydrated. After normal labs, exam, IV hydration, she was ready for discharge. I always have one of the Spanish speaking nurses help me with history and discharge instructions, but this time we were waiting for someone from upstairs to come down and interpret. I was doing a last check exam and I started the discharge info in my Spanish. I was trying to tell her to use the suppository every 12 hours if she was vomiting. She kept looking at me with a very confused look. I repeated a couple time “Tomo esta supositorio….. then I remembered I was telling her I take a suppository instead of instructing her to take it. Tomo instead of Toma. Just one letter can get you in trouble. I'm sure she wondered why I would need to tell her about my personal habits.
I understand now as a slang this could mean "up yours"
The interpreter arrived and bailed me out.
Taking German in HS and French in college in Illinois did me a lot of good. I wish I'd known I would end up in California where Spanish can be very useful.
Warning, this page is meant only for an older, more mature audience.
I can not be responsible for recurring
unpleasant recollections of images created here.
This page is part of a decades long study of unusual human behavior,
often involving items such as a cucumber, soda bottle, electronic device, spray can, insects, a supposed large member, and use your imagination.

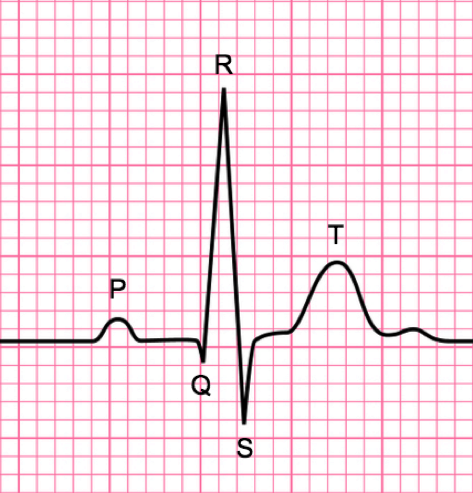
In the ER our job was to resusitate. Heart attacks, strokes, trauma.. we would do whatever necessary to get the heart beating again. We usually didn’t have to make a judgement on if it was the right thing to do. However, getting a pulse and BP back, getting them up to the ICU didn’t necessarily mean you saved a life. They might never wake up or if they did, the patient may be severely disabled. Sometimes patients would be in the ICU on ventilators for weeks or months and then crash and die. Sometimes patients would recover completely and walk out of the hospital. There was no way to predict.
Sometimes the decision on ER work was obvious. Head injuries with brain tissue lost. Long field CPR times, fixed and dilated pupils, flatline EKG, hypovolemic arrest. Cardiac arrest from blood loss was difficult to survive even with the most vigorous NS/blood infusions, interventions. Even with cracking the chest and cross-clamping the aorta and open cardiac massage. This came into use during my career, although the procedure was also known as starting the autopsy.
Many times patients were brought in dead and they stayed dead,
despite doing all the right things.

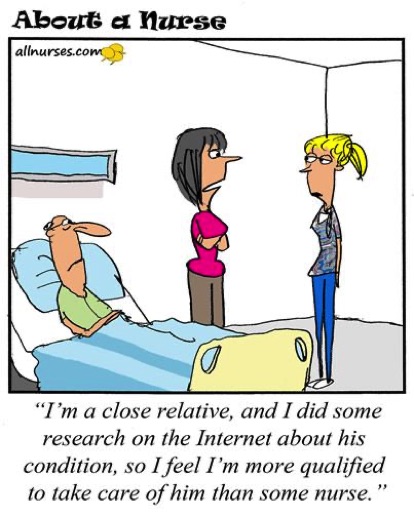
Of course Nurses are welcome,
I know better than to get on a nurse's bad side.






The question would be whether he wanted it removed or just have the batteries changed. The ER would have to start stocking various types batteries. I got it out and he took it home.
Some of the silliest cases are the most memorable.
There was the guy in room 6 that had ringing in his ear.
I was looking in his ears and I heard the ringing. Go figure. Turned out it was a low battery on his wristwatch.
There was one night we had a paramedic unit come with a hysterical man holding his hand over his left ear and thrashing about. He was screaming and not making sense. Apparently he just woke up this way. I got his hand down and with the otoscope got a look. What I saw was an insect wiggling around in his ear canal, right against the tympanic membrane. I squirted Xylocaine in his ear stop the insect movement. Then I could pull it out with a forceps. At first I thought a cockroach, but with a better look and a book check it turned out to be an earwig.
There's an old wives tale, a long standing myth, that earwigs climb into the ear canal at night and then burrow into and eat the brains of humans, and laid their eggs there.
Apparently, actually getting an earwig in your ear is extremely rare.
I should have saved the critter for a display case.
The word wig was derived from the old English word for insect.
The ears and the nose are popular places for youngsters to store things, like small toys, beads, jelly beans, seeds, nuts, popcorn. Think of some small object, it has probably been stuck up or in.
Swallowing things is also a popular pastime
and that has made for some great X-Rays
Papoosed




Big Guy

This happens to be one of my grandsons, and no, BaBa and YaYa didn't have the boys at the time of ingestion.
This turned out to be small change
Two shiney pennies.
You'll be pleased to know they were retired from general circulation.
A person coming through the ER door could be having
the worst day of their life,
the most embarrassing day of their life,
or the best day of their life.
Often they won’t know which until the ER crew has done its work.
.
My Grandson had money coming out the Wazoo
In the "Old Days" Emergency Medicine wasn't a recognized speciality. Hospitals might have the rule that to be on staff a doc had to do a shift in the ER every month or two, unless you could get someone to do it for you. Theoretically, a cardiolgist might be called on to deliver a baby or an orthopedist would treat an MI.
EM was becoming a speciality as I started work,1974. I finished my internship and the next night started work in a community ER. The American College of Emergency Medicine was formed, and medical schools included EM in their programs. I went to dozens of EM conferences and continuing educational programs.
I must admit they were in ski or beach country.
Dubious Award for Persistence
for the "Longest Active Tenure in the Same ED"
Nobody else in the country was as sedentary.
When you're having so much fun, working with people just as crazy as you are, why would you want to leave.
I wonder if anyone has broken my record of 28 years.
I've never had to go to an ER as a patient, although I've gone in to the ER maybe 7,000 times, maybe 180,000 patients. Fortunately I was never sued. I know guys who did, who had done all the right things but there was still a bad outcome. The staff has been spit on, bled on, vomited on, punched, grabbed, groped, had a gun fall on the floor as a patient was turned over, had gang fights in the ER, had maggots spill out onto the floor from a wound, had a guy on LSD running around the ER with a knife, taking care of patients who are in handcuffs and not very cooperative, dealing with a child abuse case, telling a family of a loved one's death, and perhaps the worst, having to see an infant or child that couldn't be saved. It's usually a very rewarding job, but I know the stress that the staff goes thorough at times. I've seen nurses in tears after an especially bad case, but they had to get back to a busy, backed up ER.
It's hard not to take some of it home with you.
A part of the job was talking with the anxious family members in the “family room” and tell them their loved one is alive and being admitted. I always took a nurse with me, so that I could excuse myself and get back to work, but have the nurse be with the family for more questions, consoling, something they were great at.
Unfortunately many trips to the back room were to tell family that their loved one had died. “I’m sorry. We weren’t able to revive him. His heart was too damaged. He’d been without a heart beat and oxygen to his brain for too long. He’d lost too much blood”.
Usually lots of tears and screaming. I recall one case, a gunshot victim. where the room was full of upset people. On entering the room, everybody flooded me with questions. The nurse helped me find the closest relative, the mother. I sat with her and told her softly that her son had passed away. He came into the ER with a gunshot wound to the chest, it had hit his heart and we were unable to resusitate him. One of the men in the room confronted me as I left the room and was extremely upset and yelling. He punched the wall next to me and made a fist sized whole in the sheet rock.
He also sustained a boxer’s fracture (5th metacarpal head fx) which we treated when he calmed down.
A Good Trauma Room Memory
I recall a bartender brought in code 3 with a gun shot wound to the head. He had been shot at work, in a hold up. As they brought him in, he was sitting up on the gurney and talking with a small hole mid forehead, complaining of some head pain. We started the trauma workup, labs. The skull XRay showed a small bullet midline at the back of the calvaria.
It apparently had entered his forehead and tracked midline in the median sulcus without doing much damage. A neurosurgery admit.
I later heard he did well after surgery.



As a sign of how long ago I started work, the nurses then wore white dresses, white stockings and nurse's hats.
Of course during the generation before me the nurses would stand up when a doctor came in the room.
Not My Job


I'm not sure what this means

Cheryl



“Doctor Suffers Concussion
During Pelvic Exam” .
It’s incredible the medications that are advertised on TV these days. In the “old days” we just had “Plop,Plop,Fizz, Fizz, Oh What a Relief it is!!” for Alka Seltzer, or “Morning Backache…Ache…Ache” for Doan’s Pill.
Drug reps used to visit docs to promote new meds, give them samples and toys. Now there’s a host of frequent commercials for drugs, that includes about 30 seconds describing the drug and 2 minutes of a very rapid talk warning of the side effects. At the end of the commercial, you have no idea what it’s for. Just a few: Ozempic, Afezza, Prevagen, Cosiquin, Newlastin, Eliquis, Fasenra, Humira , Repatha, Xarelto, Farxiga, Cosentyx, Chantix, Lyrica and Xeljanz, Emgality, Jardience, Trulicity, Truvada
(The United States and New Zealand are the sole countries worldwide that allow direct-to-consumer (DTC) pharmaceutical advertising).
I can just imagine working in an ER where the patient comes in having Googled his diagnosis and found his treatment on the TV. They even got a second opinion on Yahoo. It's all done for you.



Below is a YouTube link to a Saturday Night Live skit from years ago promoting Rectix. One might say it's in bad taste, gross, inappropriate, vulgar, insensitive. All true. But if Rectix did exist, I wouldn't be surprised if it generated ER visits. It's small compared to a cucumber, but a cucumber doesn't vibrate.

A suspected Covid-19 male patient is lying in bed in the hospital, wearing an oxygen mask over his mouth and nose. A young student female nurse appears and gives him a partial sponge bath.
"Nurse,"' he mumbles from behind the mask, "are my testicles black?"
Embarrassed, the young nurse replies, "I don't know, Sir. I'm only here to wash your upper body and feet."
He struggles to ask again, "Nurse, please check for me. Are my testicles black?"
Concerned that he might elevate his blood pressure and heart rate from worrying about his testicles, she overcomes her embarrassment and
pulls back the covers.
She raises his gown, holds his manhood in one hand and his testicles gently in the other.
She looks very closely and says, "There's nothing wrong with them, Sir. They look fine."
The man slowly pulls off his oxygen mask, smiles at her, and says very slowly,
"Thank you very much. That was wonderful.
Now listen very,very, closely:
"Are - my - test - results - back?"
So one question one might have after skimming this page is, why would anyone want to work an ER. The crew signs up for a unique speciality. There is no predicting what might happen at any moment. There's a baseline of visits, the chest/abd workups, the fevers, ortho, lacerations. And then there's the chaos. The adrenalin. A team jumps into action, each member with a different skill set. It's a working condition that generates great friendships.
You receive immediate feedback on your efforts. With each procedure, each med given, the results dictate your next move. When you're able to bring a patient back and into surgery or up to the ICU, it's very rewarding. But you have to get used to the fact that many patients are beyond saving.

Fellas, Do Not sit naked in plastic lawn chairs.
Just when you thought you've seen everything.
This would be a memorable ER case.
What would the Paramedic ringdown be like?
Inbound code 3 with "Acute Testicular Entrapment"
One of our ER nurses would respond back
"One Ball or Two"